When should I get an MRI of my back?
When should I get an MRI of my back? https://phoenixspineandjoint.com/wp-content/uploads/2021/04/Layer-5-1-972x1024.png 972 1024 Phoenix Spine & Joint Phoenix Spine & Joint https://phoenixspineandjoint.com/wp-content/uploads/2021/04/Layer-5-1-972x1024.pngMagnetic resonance imaging (MRI) is a crucial tool in helping us get rid of pain coming from your back. Since there’s no radiation or risk to an MRI almost everyone with back pain would like to have one to get a good picture of what is going on inside them. But when should you really have an MRI? The question is really an important one, as studies have shown that having an MRI at the wrong time can lead to unnecessary procedures and bad results.
The right time to have an MRI is either now, or after waiting 6-12 weeks (about 3 months) for things to get better on their own. The decision between now and weeks from now depends on three things: 1) whether you have red flags; 2) the type of pain you are having; and 3) how long you have been suffering. In this article we will discuss each of these issues so that you will know when the time is right to have an MRI of your lumbar spine, and how your doctors will use that information. And if you need help getting an MRI you’ll get a way to contact us to help with a prescription and the arrangements.
Have an x-ray already and want to know what it means?
We can help. To sart show us your x-ray or MRI.
Click here to upload a copy, or send us a picture
There are several conditions in which an x-ray followed by an MRI should be done now. These conditions are called red flags because they are warning the pain you are having may be serious. The red flag conditions which alert doctors to get an MRI right away are: trouble controlling your bowels or bladder; numbness or weakness in the legs that prevents you from functioning normally; as well as history, signs, or symptoms of cancer or infection.

Assuming you have no red flags, then MRI of the low back is still appropriate now if you have leg (not back) pain for three weeks AND you are preparing to have an epidural injection for nerve root pain caused by a herniated disc. The MRI of your back is the roadmap the doctor will follow to do the epidural injection. The injection is done in an ambulatory surgery center or office to avoid the risks of hospitalization. In this picture regular nerve roots are shown in yellow; while the nerve roots affected by the transforaminal epidural injection are shown in blue. The injection is done with a thin needle and takes only a few minutes. Rarely patients have numbness or weakness for a short time after epidural injection so you cannot drive yourself. Sedation is not mandatory for epidural injection but can be arranged at your request.

Epidural injection is a great way to reduce pain for a couple of days; however, epidural injection does not change the need for surgery. Think about it: people have epidural injections for pain control during childbirth, but having an epidural injection does birth the baby, the mother must do that. Similarly, epidural injection does not make a herniated disc go away, only healing over time or a surgeon can do that.
By now you can see how this works. If you have no red flags, and you did not get an MRI in preparation for an epidural injection, then you may still need an MRI of the back if conservative care is not effective after 6-12 weeks (about 3 months). The four most common problems that may show up on an MRI at that point are 1) spinal stenosis; 2) herniated disc; 3) facet joint arthritis (spondylosis), or Degenerative disc disease.
Have an x-ray already and want to know what it means?
We can help. To sart show us your x-ray or MRI.
Click here to upload a copy, or send us a picture
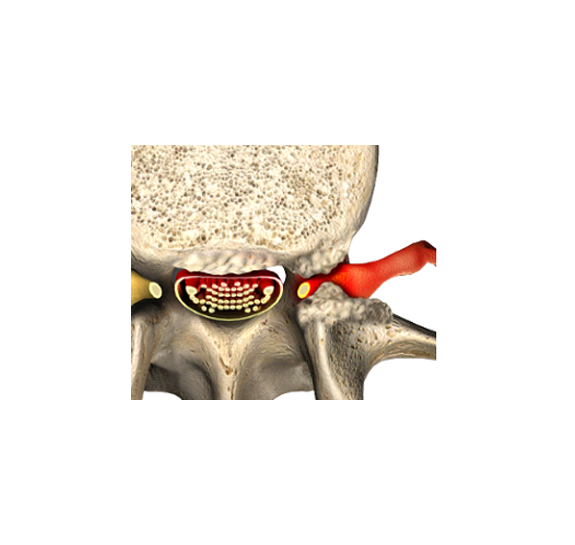
Stenosis is a ten-dollar word for narrowing. Spinal stenosis is suggested by an x-ray, but to be sure you must undergo MRI. There are three flavors of Spinal stenosis: narrowing of the spine in the middle, or of one of the small passages where the nerve root exits the spine, or along the outside edge of the spinal canal.
In this picture the nerve roots are shown in red as they are squeezed leaving the spinal canal. You may notice that right behind the nerve root is the facet joint. Just like the knuckle joints in your hands, your facet joints enlarge as you grow older. The enlargement of the facet joints narrows the hole the nerve root comes through and pinches the root. Surgery to open the hole, or foramen, is technically called foraminotomy, but in practice is usually referred to as laminectomy.

Central spinal stenosis causes compression of all the nerve roots in the spinal canal. When you walk the nerve roots cannot get enough oxygen so people with spinal stenosis feel numbness and tingling running down their legs. Spinal stenosis is progressive. Once you have it you only get worse. If the condition goes on long enough you would end up paralyzed, incontinent of urine, and unable to have sex.
The roof of the spinal canal is the lamina bone; if you want to make room in the spinal canal you raise the roof. When the spinal canal is too narrow you can open it up by raising the roof and removing the lamina bone. This is called lumbar laminectomy. Both foraminotomy and lumbar laminectomy surgery are done as an outpatient in an ambulatory surgery center by a spine surgeon. The surgery takes an hour and can be done in a minimally invasive fashion through an incision that is less than an inch. You should be up and walking 90 minutes after surgery, and ready to return to light duty work 1-2 weeks later. The pain in your legs is usually gone when you wake up.
If you have an MRI in preparation for an epidural injection and it demonstrates a herniated disc, then there is a 94% chance that your body will heal the herniation without surgery within 12 weeks (about 3 months). However, if you have unbearable pain, or functionally limiting numbness or weakness then microdiscectomy surgery is necessary.
Have an x-ray already and want to know what it means?
We can help. To sart show us your x-ray or MRI.
Click here to upload a copy, or send us a picture
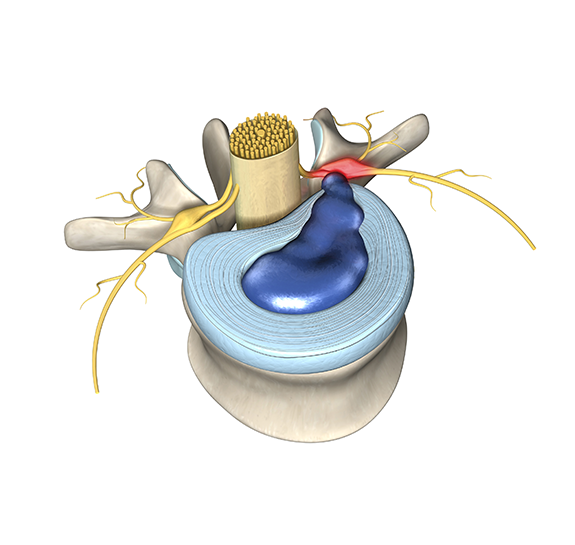
Although rare, the disc itself can become painful. Over the years injuries to a disc can add up, and the body is simply unable to heal the disc properly. This degenerative disc disease causes disc space collapse and can become painful in a of themself. In this picture you can see the disc (purple) has collapsed, and the spinal bone next to the disc is red with inflammation. This inflammation can spill out an affect the adjacent nerve roots. These chances can also be seen very well on MRI of your back.

If your disc is the source of your pain the only removing the disc can remove your pain. Once the disc is removed something must replace it. The surgery to remove and replace a disc is called spinal fusion. Spinal instability and spondylolisthesis with stenosis are two other conditions which require an MRI for evaluation and can lead to the need for spinal fusion.
Seem complicated? It is. If you want to talk it over with someone, or need help obtaining an MRI then please contact us. There is no charge for speaking to one of our highly trained and knowledgeable staff. We’re here to help.
- Post Tags:
- Pg - Epidural injection
- Posted In:
- Herniated Disc With Sciatica
- Low Back Pain
- Stenosis