When should I get an MRI of the knee? It depends whether you have arthritis, ACL or meniscus tear.
When should I get an MRI of the knee? It depends whether you have arthritis, ACL or meniscus tear. https://phoenixspineandjoint.com/wp-content/uploads/2020/11/Layer-1-1-1024x683.png 1024 683 Phoenix Spine & Joint Phoenix Spine & Joint https://phoenixspineandjoint.com/wp-content/uploads/2020/11/Layer-1-1-1024x683.pngWhen should I get an MRI of my knee?
Magnetic resonance imaging plays an especially vital role in helping us to help you get rid of your knee pain. But when should you get an MRI of the knee? Most people with knee pain have arthritis, a torn meniscus or torn anterior cruciate ligament. Arthritis shows up on a plain x-ray; but it takes MRI to know if you have a torn ACL or meniscus. That is why you should always have an x-ray before having an MRI: even if your problem does not show up on x-ray, your orthopedic surgeon will need to stage the degree of arthritis in your knee to develop the right treatment plan. If your problem is serious, you need an MRI and doctor visit emergently, which means today. But for most people MRI can wait; how long depends on whether you are over 55, and what your x-ray shows.
Have you had an x-ray of your knee and are not sure if you need an MRI? If you can’t walk on it or you’ve had pain for more than 3 weeks despite taking anti-inflammatories (Ibuprofen, Aleve) then you probably need additional care. We can help your sort it out. Complete the form near the bottom of this page which allows you to upload a copy of your x-ray.
To figure out if you need an MRI scan, a little background is in order.
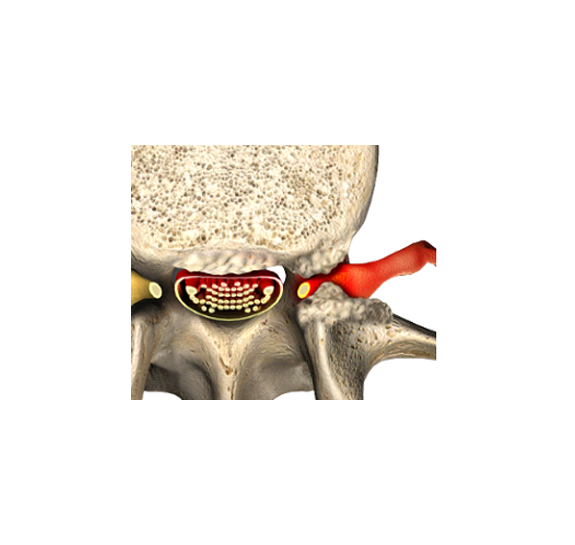
Each meniscus is a horseshoe shaped piece of cartilage between the thigh and shin bones. In this picture, looking from the front of the knee, you can appreciate how the thigh bone rests on the meniscus which functions as a cushion. The meniscus both cushions (absorbs) shocks in the knee and prevents the bones from touching and grinding against one another as the knee moves. A torn meniscus causes clicking, popping, and locking of the knee. Because the meniscus is made of cartilage, and cartilage does not show up on x-ray, a torn meniscus will not show up on x-ray. Luckily, however, a torn meniscus lights up and is shown clearly on MRI.

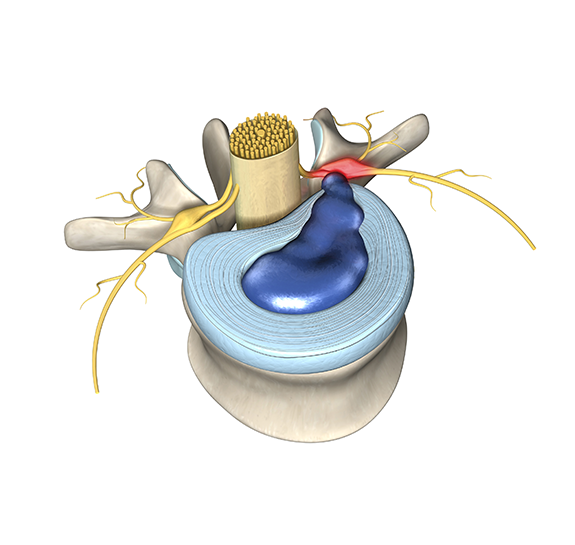
The anterior cruciate ligament (ACL) supports the knee by preventing the thigh bone from sliding forward on the leg bone. In this picture you see the knee from the back, and it is bent. The thick, strong ACL is a band that starts on the thigh bone and finished in the shin. We think of the ACL as being torn suddenly while playing a sport, but tears are often the result of gradual wear. When the ACL is torn in a sports injury you feel a pop and the knee gives out making it hard to walk. When the ACL tears more gradually there is often no specific moment or pop; knee pain and a sense that your knee cannot hold your weight comes on gradually. A ligament, like cartilage, does not show up on x-ray; therefore, a torn ACL is best seen on MRI and does not show up on x-ray.

Arthritis is the result of inflammation on the knee. This can occur due to trauma, gradual degeneration of the smooth cartilage in the knee joint (osteoarthritis), or due to an underling problem (rheumatoid arthritis). Arthritis causes thinning of the cartilage in the joint, rough surfaces, and can even result in loose bodies of cartilage floating in the fluid of the knee joint. All these changes in the knee due to arthritis can be seen on MRI; however, a knee x-ray is a valuable tool for your orthopedic surgeon to assess the overall stage of arthritis in your knee.

How do you know if your knee problem is serious? A knee problem is serious if you have any red flags (sudden onset of pain so severe you cannot walk; deformity of the knee; a red, hot, swollen knee; history of cancer; unexplained weight loss; blood in your urine, stool, or vomit) then the problem could be serious, and you need an urgent evaluation. The necessary urgent evaluation includes blood work (serum WBC (White Blood Cell), ESR, CRP), examination by a doctor experienced in serious knee conditions, x-ray, and MRI imaging. As you can tell, this type of urgent examination is most often done in a hospital emergency room. Fortunately, knee problems are rarely life threatening, and most of the time the evaluation is done outside the hospital.
So, do you need an MRI of your knee? If you have any red flags, then you need an MRI right away. Since most issues get better on their own without medical treatment then if you have no red flags and are within the first 3 weeks after injury then an MRI can wait. If your knee pain is not getting better on its own after three weeks you should see a doctor. She will perform a physical examination, x-ray, and blood tests for infection. The results of these tests will decide whether you need an MRI.
If you are over 55, your knee x-ray shows signs of arthritis, and the physical exam is not suspicious for a torn meniscus or ACL, then you have arthritis and should start rehabilitation; in this case an MRI is not needed.
On the other hand, if your arthritis is not better after three weeks of rehabilitation such as physical therapy then you should try a hyaluronic acid (synvisc, euflexxa, hyalgan, monovisc, orthovisc, supartz) injection. These injections help lubricate the synovial fluid of the knee, and often relieve pain for weeks to months. If you are still severely impaired from advanced arthritis of the knee despite hyaluronic acid injection, then it is time to see an orthopedic surgeon who specializes in partial knee replacement surgery or total knee replacement surgery for muscle sparing robotic assisted partial or total knee replacement. Muscle sparing robotic assisted partial or total knee replacement surgery takes around 1 hour, is done as an outpatient to avoid the risks of hospitalization. You are up and walking on your own 90 minutes (about 1 and a half hours) after partial or total knee replacement surgery, you can walk without a walker in 1-2 days, back to light duty work in 1-2 weeks, and you are fully recovered in 3-6 weeks (about 1 and a half months).

On the other hand, if the x-ray does not show arthritis, you are under 55, your knee pain started with a specific injury playing sports, or your physical exam suggests a torn ACL or meniscus, then you need an MRI right away. If the MRI shows a complete ACL tear or some types of meniscus injuries, then arthroscopic ACL reconstruction, Meniscectomy or meniscal repair surgery by an orthopedic surgeon who specializes in Sports Medicine would be proper. Arthroscopic, ACL Reconstruction, Meniscectomy or Meniscal Repair surgery are done on an outpatient basis to avoid the risks of hospitalization. The surgery takes 1-2 hours, and you are fully recovered from surgery after a week. Depending on the type of surgery you will require an extensive course of rehabilitation which may last 6-10 months.


- Posted In:
- ACL Reconstruction
- Knee Pain
- Meniscal Tear